Abstract
Background: Women with von Willebrand disease (VWD) may experience multiple reproductive health challenges, particularly related to menstruation and pregnancy. Patient-reported experiences in this setting have not been well characterized.
Aim: To elicit patient-reported menstrual health experiences in women with VWD.
Methods: We conducted a physician-administered telephone survey of women seen at Mayo Clinic for workup and/or management of VWD. Patients were asked to discuss their diagnosis of VWD and questioned about menstrual health, contraception, and pregnancy and asked to describe how their VWD had impacted their reproductive health experiences. Quantitative data were analyzed using R (version 3.2.0). Qualitative comments were analyzed by frequency of response (specific adjectives) and general thematic elements.
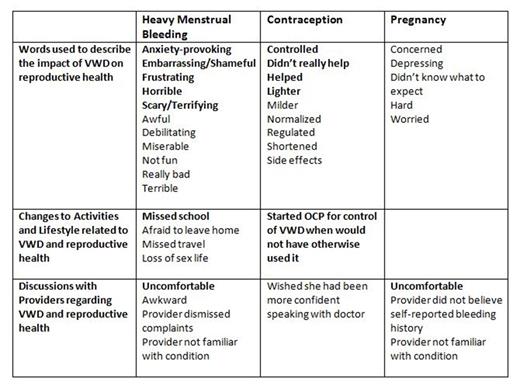
Results: Of 130 women diagnosed with VWD, 82 (63%) agreed to participate, including 58 (71%) with type 1, 9 (11%) with type 2A, 4 (5%) with type 2B, 8 (10%) with type 2M, 1 (1%) with type 2N, and 3 (2%) with type 3. 89% of women self-reported a history of heavy menstrual bleeding; for 23 (28%) this was their first bleeding event. 28 women (34%) ultimately underwent hysterectomy for heavy menstrual bleeding. Women used several forms of contraception, most commonly estrogen-containing oral contraceptives (61, 74%) and intrauterine device (9, 11%). 65 women (79%) reported at least one pregnancy. There were 200 total pregnancies (median 3 per woman, range 1-10). 142 pregnancies (71%) resulted in live term birth, 47 (24%) in spontaneous abortion (at a median of 12 weeks), 9 (4%) in a live preterm birth, and 2 (1%) in therapeutic abortion. Patients' self-reported comments are described in the Table, with responses in bold indicating the same themes were used by more than one patient. Women used primarily negative adjectives to describe heavy menstrual bleeding and reported a significant negative impact on their academic, home, and sexual lives. Despite this, women often reported that they "just dealt with it" and "thought it was normal." Regarding pregnancy and VWD, women again used primarily negative adjectives to describe their experiences. Many described pregnancy-associated bleeding events (generally postpartum hemorrhage). Overall, women reported that it was often "uncomfortable" to discuss their reproductive concerns with their medical providers (including hematologists). One woman reported that she "wished [she] had been more confident speaking with [her] doctor" and another that "it is important to be your own advocate."
Conclusions: VWD is a relatively common bleeding condition which appears to significantly impact women's reproductive health. In this qualitative interview study, women often used negative adjectives to describe their reproductive experiences as related to VWD. Additionally, many were uncomfortable discussing their reproductive health with their providers. Physicians (particularly hematologists and obstetrician-gynecologists) should be trained to recognize the impact of VWD on reproductive health and include reproductive health as part of their essential health maintenance conversations with their patients. More compassionate and informational patient-physician conversations may help to optimize reproductive health experiences and outcomes in women with VWD.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal